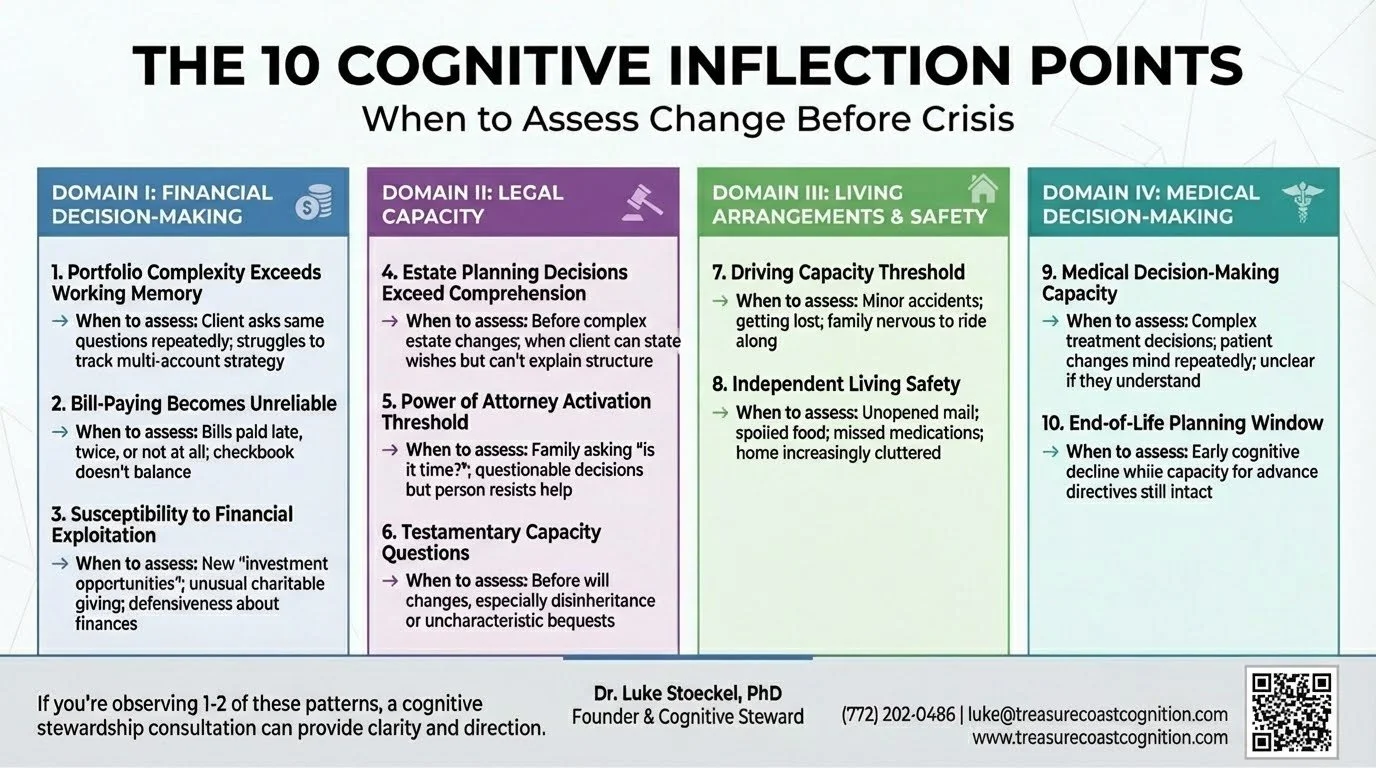
An inflection point is a moment when a relatively small cognitive change creates disproportionate risk for poor outcomes.
These aren't binary thresholds where capacity suddenly disappears. They're gradient transitions where specific cognitive functions decline in ways that impact specific real-world decisions.
The framework identifies 10 predictable decision points that most families encounter during cognitive transitions. If you recognize them early, proactive planning is still possible. If you miss the window, you're managing crisis.
Here's what to watch for:
DOMAIN I: Financial Decision-Making
1. Portfolio Complexity Exceeds Working Memory
What to watch for:
Difficulty tracking multiple accounts
Conversations with advisors require more repetition
Struggling to synthesize overall investment strategy
Increasing reliance on written summaries
The cognitive change: Working memory decline—difficulty holding and manipulating multiple pieces of information simultaneously
Why it matters: The person may still be able to discuss individual investments, but complex portfolio rebalancing, tax strategy, and multi-year planning may exceed current capacity. Without recognition of this change, they may agree to strategies they don't fully understand or resist necessary changes because they can't track the reasoning.
The decision point: Should we simplify the portfolio to match current capacity, or add oversight while maintaining complexity?
2. Bill-Paying Becomes Unreliable
What to watch for:
Bills paid late, twice, or not at all
Checkbook doesn't balance
Confusion about automatic payments
Insistence they paid something they didn't
The cognitive change: Executive function and prospective memory decline—difficulty remembering to perform future tasks and monitoring what's been completed
Why it matters: Bill-paying errors are often among the first visible signs that cognitive changes are affecting instrumental activities of daily living. Late payments can damage credit scores, duplicate payments drain accounts, and unpaid bills create legal consequences. More importantly, if bill-paying is compromised, more complex financial management is almost certainly at risk.
The decision point: Is this occasional forgetfulness that can be addressed with organizational systems, or is this evidence of declining capacity that requires direct oversight?
3. Susceptibility to Financial Exploitation
What to watch for:
Sudden interest in questionable "investment opportunities"
Difficulty ending sales calls
Charitable giving disproportionate to values or means
New "advisors" the family hasn't met
Defensiveness when questioned about financial decisions
The cognitive change: Decline in judgment, emotional regulation, and social cognition—particularly the ability to detect deception, assess risk, and resist persuasion
Why it matters: Elder financial exploitation is estimated to cost older adults billions of dollars annually, with individual losses often averaging $120,000. Once exploitation begins, it tends to escalate. Victims are often too embarrassed to report it, and by the time family members discover it, significant assets may be gone.
The decision point: Can they still manage financial relationships independently, or do they need protective oversight while preserving as much autonomy as possible?
DOMAIN II: Health & Medical Decision-Making
4. Medication Management Becomes Unreliable
What to watch for:
Medications taken at wrong times or in wrong doses
Pills remaining in organizers days after they should have been taken
Confusion about which medication treats which condition
Duplicate or missed doses
The cognitive change: Executive function and prospective memory decline affecting the ability to follow complex medication regimens
Why it matters: Medication non-adherence is associated with increased hospitalizations, disease progression, and preventable complications. For conditions like hypertension, diabetes, or heart disease, inconsistent medication use creates serious health risks. It's also an early indicator that other complex health management tasks may be compromised.
The decision point: Can medication management be maintained with organizational systems and reminders, or is direct oversight required?
5. Complex Medical Decisions Exceed Comprehension
What to watch for:
Struggling to weigh treatment trade-offs
Asking appropriate questions but difficulty retaining information
Changing mind repeatedly about treatment preferences
Physician uncertain whether they truly understand implications
The cognitive change: Decline in complex reasoning, future orientation, and ability to weigh probabilistic outcomes
Why it matters: Medical decision-making capacity is decision-specific and task-dependent. Someone might retain capacity for routine medical decisions but not for complex treatment choices involving risk/benefit analysis and uncertain outcomes. Without proper assessment, patients may make choices they don't fully understand, or family members may inappropriately override autonomous preferences.
The decision point: Can they make this specific medical decision independently, or is supported decision-making needed to ensure understanding?
6. Health Maintenance Tasks Decline
What to watch for:
Missed medical appointments
Laboratory work that doesn't get completed
Recommended screenings or follow-up visits falling through the cracks
Health conditions worsening due to lack of consistent management
The cognitive change: Executive function decline affecting planning, initiation, and follow-through on health maintenance activities
Why it matters: Preventive health care and chronic disease management require consistent execution of multi-step tasks—scheduling appointments, attending visits, following up on recommendations, and coordinating between providers. When executive function declines, these tasks can fail even when the person intellectually "knows" they should do them.
The decision point: Can health maintenance be sustained with reminders and organizational support, or does someone need to take over coordination?
7. Advance Care Planning Window
What to watch for:
Early cognitive decline but still able to discuss future care preferences
The conversation keeps getting postponed because it's difficult
Window for autonomous decision-making gradually closing
The cognitive change: Capacity for advance care planning remains intact, but progressive decline is foreseeable
Why it matters: This represents the last opportunity for the person's own voice to meaningfully guide future medical care. Once capacity is lost, families must make decisions without clear guidance from the person, often leading to conflict, guilt, and choices that may not reflect the individual's values.
The decision point: Is this the appropriate time to document preferences while decision-making capacity is intact?
DOMAIN III: Living Arrangements & Safety
8. Driving Capacity Threshold
What to watch for:
Minor traffic incidents or fender-benders
Getting lost in familiar areas
Family members feeling anxious when riding along
Slower reaction times
Defensive reactions and insistence they're "fine" despite observable concerns
The cognitive change: Possible decline in processing speed, visual-spatial function, divided attention, reaction time, judgment, or executive function—all critical for safe driving
Why it matters: Driving represents independence and identity for most adults. Loss of driving privileges is often one of the most emotionally charged transitions in cognitive aging. Yet continuing to drive with significantly impaired capacity creates safety risks for the driver and others. This requires objective assessment, not family opinion or self-report alone.
The decision point: Can they still drive safely without restrictions? Do they need limitations (daylight only, familiar routes, limited radius)? Must they cease driving?
9. Independent Living Safety
What to watch for:
Unopened mail accumulating
Spoiled food in refrigerator
Missed medications
Home increasingly cluttered or unkempt
Basic home maintenance not occurring
Safety hazards developing
Insistence they're managing fine despite visible evidence to the contrary
The cognitive change: Executive function decline affecting initiation, planning, and organization of daily tasks
Why it matters: This is the inflection point where "aging in place" transitions from preference to potential safety risk. Concerns include fall risk, medication errors, nutritional deficits, fire hazards, and vulnerability to exploitation. However, moving someone from their home prematurely can accelerate cognitive and functional decline and significantly impact quality of life.
The decision point: Can safety be maintained at home with appropriate supports, or has capacity declined to the point where a more structured living environment is necessary?
10. Social Isolation and Support System Erosion
What to watch for:
Decreasing engagement with friends and community
Not returning phone calls
Declining social invitations
Forgetting social commitments
Informal support network no longer in place
The cognitive change: Executive function and social cognition changes that make maintaining relationships more effortful, combined with reduced initiation and follow-through
Why it matters: Research indicates that social isolation is associated with accelerated cognitive decline, increased vulnerability to exploitation, and loss of the informal safety net that often identifies problems early. Without regular social contact, dangerous situations can develop undetected. Isolation may also increase dependence on whatever limited relationships remain—potentially increasing exploitation risk.
The decision point: Is the current level of social engagement adequate for safety and well-being, or does structured social support need to be introduced?
What to Do With This Framework
For Families
If you're noticing changes and wondering "is this normal aging or something more?"—that awareness is important.
Don't wait for crisis. Don't wait for formal diagnosis.
Consider these questions:
Is your parent managing finances and medications reliably?
Are health decisions becoming difficult to navigate independently?
Is driving safety becoming a concern?
Is independent living creating safety risks?
Is their support system diminishing?
If you're observing difficulties in 1-2 of these areas, it may be appropriate to seek professional assessment.
For Physicians
Routine brief cognitive screening can detect dementia but doesn't assess functional capacity for specific real-world decisions.
When patients are facing major medical or financial decisions, or when you observe functional decline in health management despite normal screening results, consider referral for comprehensive assessment including decision-specific capacity.
For Wealth Advisors
When you observe:
Portfolio management discussions requiring more repetition than previously
Uncharacteristic investment decisions
Difficulty tracking multiple accounts that were previously well-managed
Increased reliance on your recommendations without apparent understanding
Family members expressing concerns
Consider: Does my client's current cognitive capacity match the complexity of their portfolio and financial decision-making requirements?
From Reactive to Proactive
The traditional approach to cognitive aging is reactive: wait for crisis or formal diagnosis, then respond.
The 10 Cognitive Inflection Points framework enables proactive stewardship: identify specific decision points when comprehensive assessment should inform planning, intervene before crisis occurs, and navigate transitions strategically while preserving autonomy.
This framework serves:
Families - by transforming vague worry into specific, observable indicators and actionable steps
Physicians - by connecting brief cognitive screening to functional decision-making capacity assessment
Wealth advisors - by matching portfolio complexity to client cognitive capacity and identifying when oversight may be needed
The individuals themselves - by preserving autonomy where capacity exists while providing appropriate protection where capacity is declining
What Cognitive Stewardship Provides
Think of it as proactive planning for cognitive health, analogous to how you might work with a financial advisor for wealth management.
Just as you wouldn't wait until a financial crisis to plan for retirement, proactive planning for cognitive changes can prevent crises while preserving quality of life.
Comprehensive Assessment
Understanding current cognitive strengths and areas of change
Identifying which decisions can be made independently and which may need support
Establishing documented baseline for future comparison
Strategic Planning
Creating a roadmap informed by likely trajectory
Preserving independence and autonomy while addressing identified risks
Developing a proactive plan rather than crisis-driven reactions
Ongoing Professional Partnership
Regular monitoring as cognitive capacity evolves
Adjusting interventions and supports before crises develop
Expert guidance through one of life's most challenging transitions
The Bottom Line
Cognitive Stewardship is not about "taking over" or removing autonomy.
It's about providing clear information and strategic guidance so families can make informed decisions together while respecting the individual's remaining capacity and preferences.
If you're observing difficulties in 1-2 of these areas, you may be in the window where proactive planning can still make a meaningful difference.
Ready to learn more?
Schedule a complimentary consultation to discuss what you're noticing and whether comprehensive assessment and cognitive stewardship planning might be appropriate for your family.
Treasure Coast Cognition
Luke Stoeckel, PhD
Licensed Clinical Neuropsychologist
📞 (772) 202-0486
✉️ luke@treasurecoastcognition.com
🌐 www.treasurecoastcognition.com
Serving families in Vero Beach and throughout Florida's Treasure Coast
© 2025 Treasure Coast Cognition LLC. All rights reserved.